Regulation of Cardiac Activity:
Normal activities of the heart are regulated in an essential or natural way, meaning it is autoregulated by specialized muscles or the nodal tissue, therefore the heart is called myogenic. A special neural center in the medulla oblongata can moderate the cardiac function through the autonomic nervous system (ANS).
Neural signals can increase the rate of heartbeat through the sympathetic nerves, the strength of ventricular contraction and thereby the cardiac output. On the other hand, parasympathetic neural signals (another component of ANS) decrease the rate of heartbeat, the speed of conduction of action potential and thereby the cardiac output.
Adrenal medullary hormones can also increase cardiac output. The accelerator nerve of the sympathetic nervous system increases heart rate and the vagus nerve of the parasympathetic nervous system decreases heart rate.
Conducting System of Heart (Rhythmicity):
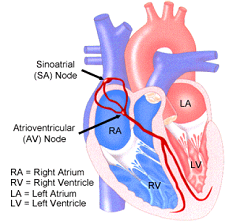
- Although the heart is a single muscle, it does not contract all at once. The contraction spreads over the heart like a wave, beginning in a small region of specialized cells in the right atrium called the Sino-Atrial Node (SAN). This is the hearts natural pacemaker, and it initiates each beat
- The impulse spreads from the SAN through the cardiac muscle of the right and left atrium, causing both atria to contract almost simultaneously.
- When the impulse reaches another special area of the heart, right in the centre of the septum, known as the Atrio-Ventricular (or AV) Node, the impulse is delayed for approximately 0.2 s. This allows time for the ventricles to fill completely.
- The AV Node relays the electrical impulse down the septum, along the Bundle of His, to the base of the ventricles. The ventricles then contract simultaneously, from the bottom upwards, thus allowing them to empty completely with each beat.
- The heartbeat is initiated by the Sino-Atrial Node and passes through the Atrio-Ventricular Node, remaining at the same rhythm until nerve impulses cause it to speed up or to slow down. Unlike other muscles, it does not require a new nerve impulse for each contraction.
Heart Beat and Pulse
- Pulse is the pressure wave that travels through the arteries after each ventricular systole. Pulse can be felt in any artery that lies near the surface of the body. During each stroke ventricle pump 70 ml of blood.
- The radial artery in the wrist is most commonly used to feel the pulse. One heartbeat creates one pulse. Hence pulse rate gives the count of heart rate.
- For most people, their resting heart rate is between 60 and 80 b.p.m. During exercise that can increase to as many as 200 beats per minute for an athlete; for the rest of us, 150 b.p.m. is about all we can safely manage.
- Pulse rate is higher in children, females and in standing position. It is lower in adults, males and in lying position. It increases with disturbing emotional state.
Regulation of Heart Beat:
The activity of the circulatory system is constantly changing according to the body’s demands, hence the heart rate is adjusted accordingly. It is achieved by two types of the control system, one is nervous and the other is chemical.
Nervous Control of Heart Rate:
The nerves controlling the heart are of both types viz. parasympathetic and sympathetic. Within medulla oblongata of the hindbrain, a controlling centre called cardio inhibition centre is present. This centre sends inhibitory impulses continuously through the vagus nerve to the heart. the nerve fibres are sent to SA node, AV node and bundle of His.
The cardiac acceleration centres are situated on lateral horns of the spinal cord in the upper thoracic segments. From this centre, preganglionic nerves arise and enter the heart. This centre is responsible for the acceleration of the heart rate.
These two activities of inhibiting and accelerating of heart rate control the heart rate.
Chemical Regulation of Heart rate:
Besides nervous stimuli, some chemical stimuli regulate the heart rate. low pH or high CO2 level and high temperature accelerate the heartbeat. Thyroid hormone thyroxine produces a faster pulse and higher blood pressure. In low quantity adrenaline secreted by adrenal glands causes acceleration of heart rate producing dilation of arteries and low blood pressure. In a higher quantity, it increases heart rate. Vasopressin secreted by the pituitary gland produces vasoconstriction.
Elecrocardiogram (ECG):
ECG is a graphical representation of the electrical activity of the heart during a cardiac cycle. Activity stimulates the heart to contract more vigorously than it does when the body is at rest. The ECG apparatus sensor measures cardiac electrical potential waveforms (voltages) produced by the heart as its chambers contract.
The ECG is not a direct measure of heart muscle activity. However, a comparison of the ECG measured during rest and the ECG measured after mild exercise may indicate the changes that take place in the cycle of heart contractions due to activity.
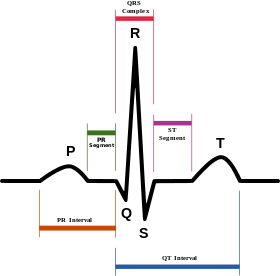
Each peak in the ECG is identified with a letter from P to T that corresponds to a specific electrical activity of the heart. One part of a typical ECG is a ‘flat line’ or trace indicating no detectable electrical activity. This line is called the Isoelectric line. Deviation from this line indicates electrical activity of the heart muscles.
P – wave: It is a small upward wave representing impulse generated by SA node. It causes atrial depolarization resulting in atrial contraction.
QRS Complex: It is a small upward wave representing impulse generated by SA node. It causes atrial depolarization resulting in atrial contraction. After a return to the Isoelectric line there is a short delay. Then ORS complex begins as downward deflection, continues as large upward triangular wave and ends as a downward wave. It shows spreading of impulse from SA node to the AV node, then to Bundle of His and Purkinje fibres. It causes ventricular depolarization resulting in ventricle contraction.
T – wave: After a short period of time the chemical ions that have been involved in the contraction migrate back to their original locations. The movement of these ions generates an upward wave that then returns to the Isoelectric line. It is a broad upward wave which represents ventricle repolarization resulting in ventricle relaxation.
Terminology in Cardiac Activity:
Refractory Period:
Once the cardiac muscle has begun to contract it can not respond to any other stimulus (whatever may be its intensity) until it begins to relax. This is known as the refractory period. During this period the second contraction can not be initiated.
This prolonged refractory period gives sufficient time gap for cardiac muscles to relax. Due to this arrangement cardiac muscles never fatigued or in a state of sustained contraction (tetanisation).
Stroke Volume:
Stroke volume (SV) is the amount of blood ejected by a ventricle during each systole. Stroke volume is related to the stretch on the heart before it contracts (preload), the forcefulness of contraction (contractility) and pressure that must be exerted before ventricular ejection can begin (afterload).
A healthy heart pumps out all the blood that has entered its chamber during the previous diastole. At rest, this is 50-60 % of the total volume because 40-50 % remains in the ventricle after each contraction.
Hence, Stroke Volume (SV) = End Diastolic Volume (EDV) – End Systolic Volume (ESV)
Cardiac Output:
The amount of blood flowing from the heart over a given period of time is called the cardiac output. It depends on stroke volume and the heart rate.
Thus cardiac output (in litre per minute) = Stroke volume (SV) ( in mlitre) x Heart rate (in per minute)
Factors affecting cardiac output are ventricular end-diastolic volume, venous return, the strength of myocardial contraction, blood volume, autonomic nerve stimulation, activity and exercise, emotional state, gender, age, body temperature, baroreceptor reflex. The rise in cardiac output ensures an enhanced supply of oxygen and nutrients to contracting muscles. During sleep, cardiac output falls.
Cardiac Reserve:
The ratio of maximum cardiac output a person can achieve to cardiac output at rest is called cardiac reserve. An average value is 4 to 5. The top athlete may have the value up to 8. People suffering from heart diseases have a low or negligible cardiac reserve. Hence they are fatigued very easily during even simple daily work.