In this article, we shall study the female reproductive system in humans.
Human Reproductive System:
Puberty means the changes that occur in boys and girls as they grow up. In this period the maturity of human sex organs begins. Most of these changes occur between the ages of 10 to 14 years. These changes are brought about by certain hormones. During puberty, the body grows rapidly, and both primary and secondary reproductive organs grow and become mature. Along with these changes, secondary sex characters also start appearing.
In males, primary sex organs are male gonads also known as testis. testis produce male gametes (male sex cells) also called sperms or spermatozoa. In females, primary sex organs are the ovary. Ovary produces an ovum, plural: ova (female sex cells) also referred as eggs. The secondary sex organs are different in males and females. They include reproductive ducts for transporting gametes and accessory gland which help reproduction.
In males, sexual maturity is attained at the age of 13–14 years and in females, at the age of 11–13 years. Puberty ultimately leads to a stage when the child becomes an adolescent. The World Health Organization (WHO) defines adolescence as the period from 10 to 19 years of age characterized by developments and changes in physical, psychological, and social areas.
During adolescence, the secondary sexual characters that develop are as follows:
- In males: deepening of the voice, widening of shoulders, muscular body, the appearance of beard and moustache, the growth of axillary and pubic hair, enlargement of external genital organs.
- In females: the growth of axillary and pubic hair, widening of pelvis and hip, enlargement of breasts (mammary glands) and initiation of the menstrual cycle.
The Stages of Human Reproduction:
Human shows sexual reproduction and the changes in the body takes place for viviparity. viviparity means the development of the embryo inside the body of the parent, eventually leading to live birth,
- Formation of gametes (Gametogenesis)
- Changes in the female body to facilitate the entry of sperms during copulation.
- The fusion of gametes. (Fertilization).
- Development of Zygote. (Embryology).
- Production of milk for the nourishment of young ones.
- Hormonal coordination by pituitary glands and gonads.
Human Fenmale Reproductive System:
The female reproductive system is divided into external and internal genitalia.
Female External Genitalia:
The ‘Vulva’ or the female external genital organs are those genital organs that are present on the surface of the female body and are also known as the female sexual organs.
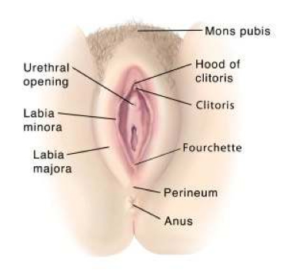
Labia majora:
These are two large longitudinal folds (on the right and left side, of the vestibule) which form the boundary of the vulva and underlying fat extending backwards from the mons pubis. They are homologous to the scrotum in males. Posteriorly they merge into the perineum in front of the anus. It almost extends up to anus. Their outer surface becomes covered with hair at puberty. But the inner surface remains smooth, moistened with the secretions from the sebaceous (Sebaceous glands are microscopic exocrine glands in the skin that secrete an oily or waxy matter, called sebum) and other glands deep inside. The labia majora also contain apocrine glands (they are exocrine glands those produce sweat). They are composed of skin, fibrous tissue and fat.
In a young girl, before the onset of menstruation, the labia majora are thinner with less fat and a fine smooth skin. Hair growth over the labia majora is one of the first signs of maturity of a young girl. In women in menopause, the labia majora becomes thinner with less fat and considerable hair loss.
Labia minora:
These are smaller and thinner lip like folds located just next to the labia majora. The labia minora is also known as the inner labia, inner lips, or nymphae. They fold and protect the opening of the vagina, the urethra, and the clitoris. Labia minora forms a small projection at their upper end which is called prepuce. Labia minora are of different sizes in different women and the two labia minora may be of different sizes even in the same woman. If large in size, one or both labia may protrude from between the labia majora. Their inner surfaces remain in contact with each other. Posteriorly the labia minora are fused together to form fourchette. The labia minora contains no fat but are highly vascular that they become turgid during sexual stimulation. They are very sensitive to touch and pressure.
Labia are very thin and delicate, they can get torn during the labour or childbirth and may cause heavy bleeding and may continue up to six weeks from childbirth.
Mons Pubis (mons veneris):
The mons pubis is a fatty region that can be found directly above a woman’s pubic bone and above the labia majora. It comprises of coarse skin and pubic hair. It Provides a woman’s body, underlying bones, and tissues, natural physical protection during sexual intercourse.
Clitoris:
It is one of the most sensitive sexual organs of a woman’s anatomy. It is located in the external area at the anterior end of labia minora. and above the opening of the vagina. It is small erectile organ. It is homologous to the penis of males. It shows the presence of erectile tissues.
It is solely designed to provide a woman with feelings of sexual pleasure and has no role in child conception.
Vestibule:
The vestibule is the part of the vulva lying between the two labia minora. It is a median vertical depression of vulva enclosing two important openings a) the external urethral opening which is a small slit-like opening just behind the clitoris and b) the vaginal opening which is a larger opening behind the urethral opening.
Hymen:
- The opening of the vagina is covered by a thin incomplete or partially occluding mucous membrane, called the ‘hymen’. In very rare cases it may be completely absent. In a condition known as the Imperforate hymen, the hymen forms a thick membrane completely covering the vaginal opening. It prevents the flow of blood and discharge during the periods and needs surgical treatment when a girl attains puberty. The hymen may break during sports or a heavy physical activity or during the initial act of sexual intercourse.
Vestibular Glands:
They are also called Bartholin’s glands. These are small pea-sized glands situated inside the vestibule on either side of the vaginal opening. These glands are homologous to the Cowper’s glands in the male. They secret lubricating fluid to lubricate the vagina and vulva. The duct from the gland to the vagina may sometimes get blocked, forming what is known as a Bartholin’s cyst. This cyst may need surgical treatment if it causes discomfort.
Breasts:
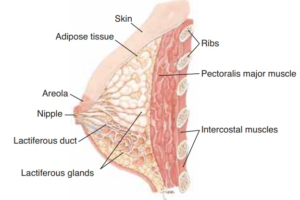
Anatomically they are known as mammary glands. These are a pair of rounded structures found in the pectoral region (chest region) on the ventral thoracic wall. They are present in both males and females. The structure of the male breast is nearly identical to that of the female breast, except that the male breast tissue lacks the specialized lobules, as there is no physiologic need for milk production by the male breast. They are well developed after puberty particularly in females. The breast does not contain muscles.
Each breast is a soft and rounded elevation. The skin over the centre of the elevation has a darkly pigmented circular area called the areola. There is a projection at the centre of areola called nipple which is erectile. These are modified sweat glands. Each breast contains fatty connective tissues and numerous lactiferous glands. It has 15 to 20 openings of lactiferous ducts which carry milk from mammary glands to nipples. Lactiferous glands dilate (become large) and form lactiferous sinuses just beneath the nipple to store the milk. The release of milk from the breast is under the control of hormones prolactin and oxytocin secreted by pituitary glands.
During pregnancy, the ducts undergo a prominent change. They branch and the terminal part develops into proper alveoli. Towards the end of pregnancy, alveoli become distended and their cells start secreting milk. After lactation period the glandular tissue returns to the resting state.
It undergoes atrophy ( waste away due to the degeneration of cells) after menopause.
Skene’s Glands:
The Skene’s gland is also called the lesser vestibular, periurethral or paraurethral glands, or the correct name of the female prostate, and are located on the upper wall of the vagina and around the lower end near the urethral opening. The glands are made of the same cells as the male prostate and are what is thought to secrete the fluid ejected in female ejaculation.
Vestibular Bulbs:
the vestibular bulbs or clitoral bulbs are two elongated masses of erectile tissues situated on either side of the vaginal opening. They are more related to clitoris than the vestibule.
Perineum:
The perineum is the less hairy cutaneous area lying between the vaginal orifice in front and the anus behind.
Female Internal Genitalia:
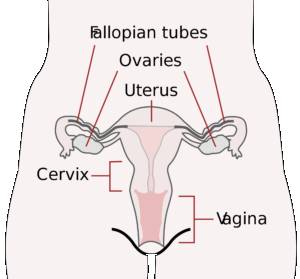
Position of Internal Genitalia (Ventral View)

Position of Internal Genitalia (Lateral View)

Internal Genitalia (Front Sectional View)

Ovaries:
Ovaries are the primary sex organs of the female reproductive system. Ovaries are oval-shaped and almond-shaped glands, which lie in the lower part of the abdominal cavity on each side of a woman’s body. The Ovaries, which rest above a woman’s Fallopian Tubes. Each ovary is suspended from the dorsal body wall by a fold of peritoneum (the mesovarium). The ovary is connected to the uterus by an ovarian ligament and is connected to the lateral body wall by a suspensory ligament.
In both the males and females, the gonads develop within the mesonephric ridge and descend through the abdomen. However, unlike the testes, the ovaries stop in the pelvis.
Functions of Ovaries:
- The Ovaries store a woman’s eggs throughout her life cycle, from birth until menopause
- The Ovaries secrete female sex hormones, oestrogen, and progesterone. These two hormones control the menstrual cycle and secondary sexual characters. These hormones can also influence a woman’s mood, sex desire, energy, and additional feelings/reactions
- The Ovaries produce an egg every month which is important for pregnancy. The process of formation of egg in the ovary is known
as oogenesis.
Structure of Ovaries:

Surface: The surface layer of the ovary is formed by germinal epithelium consisting of a simple cuboidal epithelium. This lining is continuous with the mesothelium lining called peritoneum.
Cortex: The cortex is the outer part of the ovary. The cortex contains numerous spherical or oval sac like masses of cells known as ovarian follicles (Graffian follicles) and connective tissue called stroma. is largely comprised of a connective tissue stroma. It supports thousands of ovarian follicles. Each primordial follicle contains an oocyte surrounded by a single layer of follicular cells.Ovarian follicles are in various stages of development.
Medulla: The medulla (inner part) is composed of supporting stroma and contains a rich neurovascular network which enters the hilum of ovary from the mesovarium.
Ovarian Follicles:
The ovarian follicle carries a large centrally placed ovum, surrounded by several layers of follicular granulosa (granular cells)
Folliculogenesis:
Primordial Follicles: Primordial follicles are the initial reproductive units of the ovary that occur during the fetal development. They are present in very large number ( more than 2 million). At the birth of girl child, each ovary contains 1 million oogonia and 40000 remain by the time of puberty. Of these 400-450 of these primordial follicles reach maturity during the process of folliculogenesis. Remaining oogonia degenerate. The immature ovum or primary oocyte and surrounding follicular granulosa constitute the primordial follicle.

Primary Follicles: On attaining puberty, primordial follicles start to develop rapidly into primary follicles. During this transformation, the follicular cells convert into columnar cells and go through mitotic division to form multilayered granulosa cells. The sie oocyte in primary follicle is larger than that in primordial cells.
oocyte when compared to oocyte size in primordial follicles. on maturation, a uniform membrane called zona pellucida appears between the granulosa cells and oocyte.

Tertiary Follicles: Survived secondary follicle develops into tertiary follicle which is characterised by a fluid cavity called antrum (antral follicle). The oocyte lies at the edge of a mound made up of granulosa epithelial cells known as cumulus oophorous. oocyte grows in size and completes first meiotic division. The theca layer gets organised into two layers inner theca interna (well supplied with capillaries, from lipid-rich cells) and outer theca externa (contains larger vessels).

Graafian Follicle: The tertiary follicle further develops into the mature follicle called Graafian follicle. Graafian follicle ruptures and releases the secondary oocyte (ovum) from the ovary every menstrual cycle (alternatively from right and left ovary) by the process called ovulation.

Corpus Luteum:
The ovum is shed from the ovary by the rupture of the Graffian follicle. This shedding of the ovum is called ovulation. Generally, it occurs14 days before the starting of the next menstrual cycle. After shedding primary oocyte divides and becomes the secondary oocyte. After shedding the ovum, the remaining part of the Graffian follicle is called corpus luteum (Latin: yellow body). The luteal phase is the second half of a woman’s menstrual cycle. The luteal phase begins after ovulation and continues until menstruation occurs.
The corpus luteum produces progesterone. Progesterone makes the lining of the uterus thick for implantation and is necessary to sustain a healthy pregnancy. The production of progesterone continues till the placenta begins to take over progesterone production.
Now there are two possibilities i.e. the egg (ovum) is not fertilized or egg is fertilized. Let us consider the first case when the egg is not fertilized. In this case, the corpus luteum dies and progesterone production stops. The corpus luteum regenerates and gets converted into fibrous tissue called corpus albicans (Latin: white body). When progesterone levels drop, the uterus lining stops thickening and is consequently shed during menstruation. If the egg is fertilized, the corpus luteum starts receiving HCG(human chorionic gonadotropin) from the developing embryo. HCG instructs the corpus luteum to keep producing progesterone. After ten weeks the placenta takes over progesterone production through the end of pregnancy. Hence corpus luteum lasts for maximum ten weeks.
If the corpus luteum does not produce enough progesterone (deficiency is called corpus luteum defect) to allow a pregnancy to develop then the lining of the uterus will begin to shed. The low progesterone levels in a pregnant woman may result in miscarriage.
Ovarian Cycle:
The series of changes that begins with the formation of the ovarian follicle and ends with degeneration of corpus luteum is called ovarian cycle.

Duct System:
It consists of two fallopian tubes, uterus, cervix and vagina.
Fallopian Tubes or Uterine Tubes (oviducts):
It is part of the female reproductive system which receives the egg (ovum) shed by the ovary during ovulation. It provides an appropriate environment for fertilization and transport of the egg to the uterus. It is a muscular tube about 10 cm long. Its lumen has a lining of ciliated epithelial cells. The opening of the fallopian tube is expanded into fimbriated funnel also called infundibulum that captures the ovum shed by the ovary. The infundibulum bears a number of finger-like processes at its free border called fimbriae. It shows the presence of an opening called ostium. The ciliated lining of lumen pushes the ovum towards the uterus.
For pregnancy to occur the fertilization should take place inside the fallopian tube. Ampula is the site of fertilization. To prepare for this potential occurrence of fertilization, the fallopian tubes have a healthy and nurturing lining. It facilitates the embryo to experience a safe voyage to the Uterus. Generally, embryos take several days to pass through the fallopian tubes into the Uterus but in some cases, it may take just a few hours.
Fallopian Tubes play a vital role in a woman’s reproductive abilities, hence any damage or tear to these tubes can cause infertility or conception difficulties.
Uterus (Womb):
It is a hollow muscular thick walled cavity approximately 7 cm in length, 5 cm wide and 2.5 cm thick. It is located at the midline of the pelvic cavity behind the urinary bladder and in front of the rectum. The wall of the uterus is made up of three layers the innermost endometrium, middle myometrium, and outermost perimetrium. The endometrium layer is richly supplied with blood vessels. Its innermost layer endometrium undergoes prominent cyclical changes the constitutes the menstrual cycle. Both the fallopian tubes open in the uterus. There is a sphincter muscle that closes the lower end of the uterus where it joins the vagina.
It is differentiated into a dome-shaped part above the opening of fallopian tubes called fundus. The broad upper part called body or corpus and narrow cylindrical part called cervix.
The uterus provides embryo with nurturing, safe, and nourishing environment. It is a temporary “home” for a developing fetus.
Potential Uterine problems that can negatively impact a woman’s ability to become pregnant typically include:
- Fibroid growths: They are non-cancerous growths leading to pain and bleeding
- Endometriosis: The nourishing lining is formed outside of the Uterus instead of the inner side..
- Heavy menstruation patterns: uncommonly heavy periods or frequent bleeding between periods
- Hormonal imbalances
Cervix:
The cervix is a cylinder-shaped neck of tissue that connects the vagina and uterus. Located at the lowermost portion of the uterus. It is composed primarily of fibromuscular tissue. the Cervix remains shut during pregnancy, allowing a woman’s Uterus to support the developmental processes. During delivery of the child, the cervix will open several centimetres. This opening of the cervix is called “dilation”. As the cervix opens, a woman is able to push her baby out of the Uterus and down through the Vagina.
Vagina:
It is highly collapsible and highly distensible muscular passage 8 to 10 cm long. It connects uterus to the external world. It receives penis, the male reproductive organ and spermatozoa during copulation. It acts as a duct for the passage of uterine secretions and menstrual flow. It also acts as a path for the emergence of the baby into outside world during delivery.
It has three layers of tissue: mucosa, muscle, and fibrous tissue. The mucosa layer is the smooth surface layer. Below the mucosa, the fibro-elastic muscle tissues are present. They are used for tightening and widening of the vagina during sexual activities and childbirth (labour). The fibrous tissue of the third layer helps connect the vagina to other vital structures within a woman’s body.
Vaginal bacteria (Lactobacilli) ferment the stored glycogen and makes the mucus acidic. Which prevents fungal infection.
Puberty in Female:
At puberty the internal reproductive organs reach maturity. The period is referred as menarche. It symbolises the beginning of the childbearing period.
The ovaries are simulated by the gonadotropins from the anterior pituitary and follicle stimulating hormone (FSH) and luteinising hormone (LH).